Understanding the IVF Process
In Vitro Fertilization process includes combining a woman’s eggs (oocytes) with a man’s sperm in a laboratory setting. The resulting fertilized egg (embryo) is then placed into a woman’s uterus. Below is a step-by-step explanation of the IVF process, from preparation through embryo transfer.
STEP 1: Ovarian stimulation for egg retrieval
Certain factors will need to be evaluated before a woman is deemed a suitable candidate for IVF. Once she has been approved, the first step in the process is ovarian stimulation. Naturally, a woman’s ovaries produce one mature egg for each menstrual cycle. Ovarian stimulation uses medication to increase the number of eggs produced from one to as many as twenty or more. Generally, the more eggs produced and retrieved, the higher likelihood of IVF success. To understand how ovarian stimulation medications work, one must first understand the body’s natural process for producing an egg.
Ovulation
A woman creates her lifetime supply of eggs between 5 and 20 weeks gestation (before she is born). These eggs are stored in her ovaries until she reaches puberty. With the beginning of each menstrual cycle and over the subsequent 12-16 days, a group of eggs become available for potential release (ovulation) The brain uses a combination of hormones, including follicle stimulating hormone (FSH), luteinizing hormone (LH) and estrogen to select the one egg that will be released that month (ovulation) and prepare the uterus for possible embryo implantation.
Types of Ovarian Stimulation
During IVF we amplify the body’s natural process of egg production in order to make multiple eggs available. There are several different types of ovarian stimulation protocols that can be used to accomplish this task. Choosing the correct protocol can be the single most important step in achieving a successful outcome for IVF. Drs. Marc Kalan and Nurit Winkler use their vast experience and training to choose the appropriate protocol for each individual patient. Some general categories of stimulation protocols include:
- Long Protocol with Lupron Down Regulation
- Short Protocol with GonRH Antagonist
- Short Protocol with Microdose flare Lupron
- Mini and Natural Protocols
If a woman does not release mature eggs on a regular basis, gonadotropins or clomiphene may be used in conjunction with in IVF to induce ovulation.
STEP 2. Office Visits for Monitoring
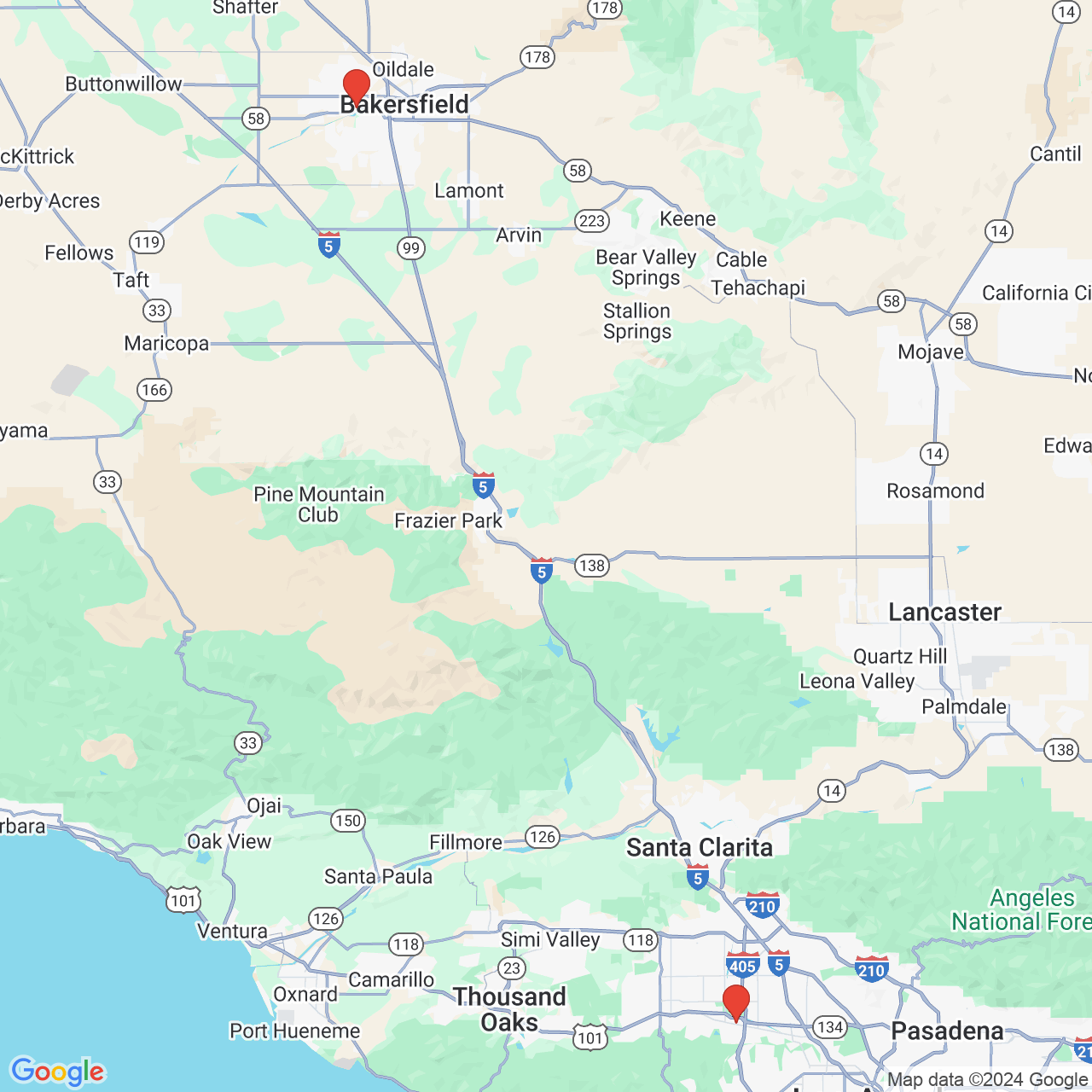
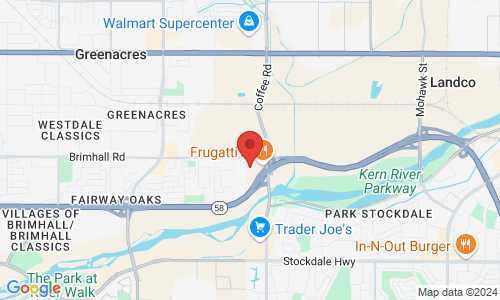
Each protocol requires a regimen of daily injections of medication (gonadotropins) to stimulate the ovaries to produce eggs. While on these medications, you will undergo monitoring at our Encino or Bakersfield office. The number of visits will vary depending on the protocol and your response to the medications. Using ultrasound and blood test, Drs. Kalan and Winkler will monitor the effectiveness of the protocol and adjust, if needed. When it appears that the egg follicles are at an appropriate, mature size, you will be instructed to take a “trigger” injection of human chorionic gonadotropin (hCG) or leuprolide (lupron) to induce the final maturation of the eggs and to prepare for the egg retrieval.
STEP 3: Oocyte retrieval (Egg Retrieval)
After successfully stimulating the body to produce eggs, a simple outpatient procedure is performed to remove the eggs from the ovaries, this is known as an egg retrieval procedure. The egg retrieval procedure is performed under conscious sedation anesthesia by an experienced and specialized anesthesiologist to ensure your comfort and safety. Assisted by vaginal ultrasound guidance, Drs. Kalan or Winkler will insert a needle into the egg follicles and remove the eggs safely. The egg retrieval process generally takes about 15-20 minutes.
STEP 4: Fertilization of the Egg
After the egg retrieval procedure is complete, the next step in the IVF process is insemination of the eggs
Traditional IVF vs. Intracytoplasmic Sperm Injection (ICSI)
In traditional IVF, eggs are exposed to sperm when they are combined in a specially designed culture dish and left to incubate overnight in the laboratory. In some circumstances, simply mixing the eggs and sperm outside the body will not result in fertilization and the production of an embryo. When there is reason to believe that fertilization may not occur with mixing, ICSI (intracytoplasmic sperm injection) is utilized to improve the chance of fertilization. Read more about ICSI below.
Laboratory Events & Milestones
After the egg has been successfully fertilized, a series of embryonic milestones unfold:
- Day 1: Pronuclear Stage
- Day 2: 4 Cell Stage
- Day 3: 8 Cell Stage
- Day 4: Morula
- Day 5: Blastocyst
These are the same steps that normally occur in nature (within the fallopian tube). We make a tremendous effort to create a laboratory environment that closely mimics that natural environment and our excellent success rates are a testament to that effort. Ultimately, a good laboratory allows embryos to grow appropriately and eventually become healthy babies.
STEP 5: Embryo Transfer
The transfer of viable embryos most commonly occurs 5 days following the egg retrieval, when the embryos are at the blastocyst stage. Drs. Winkler and Kalan can also transfer the embryos earlier of later and will discuss with you the best day to transfer the embryos and the number of embryos to transfer.
Deciding on the number of embryos to transfer depends on several variables. Age of the egg source, embryo quality, preimplantation genetic diagnosis (PGD) results, transfer day, medical history, patient preference and more all go in to the decision. Further, the American Society of Reproductive Medicine(ASRM) has published guidelines recommending the appropriate number of embryos to transfer based on patient age and history. With this in mind, Drs. Kalan and Winkler ultimately strive to work with their patients to decide on a safe and appropriate number for each individual circumstance.
The embryo transfer is an elegant and simple procedure that is designed to place the embryo(s) into a receptive endometrial environment. To begin the transfer, the patient is positioned on a specially designed bed and an empty catheter is placed in to the uterus using ultrasound guidance. Once the empty catheter is perfectly positioned, the embryology staff is instructed to load the embryo(s) into another identical catheter. The loaded catheter is then brought to the doctor who simply replaces the empty catheter with the loaded one. The embryos are then gently advanced into the uterus where they will eventually implant and begin to grow. Approximately 9 to 11 days later a pregnancy test will (hopefully) confirm that the patient is pregnant!
Additional Variations of IVF
In certain circumstances, it may be necessary to utilize one or more of the following procedures to improve the chance for the successful development of an embryo. Read more about ICSI, TESE, Assisted Hatching and Embryo Freezing:
Intracytoplasmic Sperm Injection (ICSI)
ICSI involves identifying and selecting normal appearing individual sperm. Each one is carefully loaded into a specially designed, microscopic glass needle and then precisely injected into the cytoplasm (fluid) of the egg. ICSI was initially developed to be used when there were very few or very poor quality sperm. Since then however, its use has expanded to include prior poor fertilization, low number of eggs, unexplained failed IVF or infertility and some genetic conditions.
Testicular Sperm Extraction (TESE)
In situations where a man has extremely low number of sperm or no sperm in the ejaculate (including men who have had a vasectomy or failed vasectomy reversal) it may be possible for a urologist to perform a testicular biopsy to retrieve sperm that can be used for IVF with ICSI. Los Angeles Reproductive Center works with a number of urologists in Los Angeles, CA who can perform the TESE procedure, and our embryology staff is available to work in conjunction to make sure that sperm are adequate and that the biopsy is processed appropriately.
Assisted Hatching
Assisted hatching is a procedure that helps the embryo make contact and implant into the uterine endometrial lining. The procedure of assisted hatching involves using a precise laser to create a tiny opening in the outer membrane of the embryo moments before it is transferred into the woman’s uterus. That tiny hole in the embryo’s membrane allows the embryo to more easily emerge from its outer covering (a normal part of the embryo development process), and implant in the uterus.
Embryo Freezing (cryopreservation)
Drs. Winkler or Kalan may recommend freezing some or all of a patient’s embryos. The freezing process involves rapid cooling, in liquid nitrogen, to a temperature that perfectly preserves all of the delicate structures and material within the embryo. Once frozen, an embryo can remain perfectly preserved for many years until the patient is ready to use it. At that time, using a specific thawing protocol, the embryo gently brought back to body temperature and then transferred it into the uterus.